An Overview of Thyroid Hormone Function
Thyroid hormones are essential in controlling metabolism. Below are the functions:
Source. Note about effects on cholesterol — thyroid hormones increase liver activity, so the liver filters blood faster. This decreases the amount of cholesterol in the blood. I am not entirely sure why, but here’s my guess: if the liver is busy processing blood, it will not have the energy to synthesize cholesterol at the same time. Thus, higher thyroid hormone levels lower cholesterol. Interesting tangent thought: does this mean hypothyroidism increases cholesterol and thereby increases the probability of developing atherosclerosis? A Google search tells me no… I wonder why… :(
*UPDATE: I found out that the mechanism of thyroid hormones decreasing cholesterol synthesis is through HMG-CoA reductase phosphorylation (and therefore activation) inhibition! So cholesterol cannot be synthesized! Source.
The thyroid hormone synthesis pathway is regulated by a negative feedback loop. The hypothalamus releases thyrotropin-releasing hormone (TRH), which is a tropic hormone because it affects the function of another endocrine gland. In response to TRH, which travels down the hypophyseal portal system, the anterior pituitary releases thyrotropin, or thyroid-stimulating hormone (TSH) which is also tropic. TSH acts on the thyroid gland to stimulate release of thyroid hormone (TH). There are two subtypes of TH: triiodothyronine (T3) and thyroxine (T4). T3 is the active form, and T4 is the inactive form.
Iodine is necessary for thyroid hormone synthesis. In the colloid of the thyroid follicles is thyroglobulin (Tg), whose tyrosine residues are cleaved upon combining with iodine. The follicular cells surrounding the colloid secrete Tg into the colloid. This allows formation of the TH variants. In addition to serving as a precursor to TH, Tg can store TH until release is stimulated by TSH. TSH stimulates cleavage of TH from Tg, thus freeing TH for release into the blood. Tg is recycled for further storage of TH or later synthesis of TH. Thus, Tg is like a machine that makes TH upon iodination, and releases TH into the blood when stimulated by TSH.
Thyroid hormone synthesis from the tyrosine residues on thyroglobulin molecules.
MIT = tyrosine + 1 iodine
DIT = tyrosine + 2 iodine
DIT + DIT = T4
DIT + MIT = T3
Because iodine is necessary for thyroid hormone synthesis, deficiencies of iodine can exert major effects on this pathway. An iodine deficiency prevents TH synthesis, and TSH will continue to be released due to diminished negative feedback. Basically, the body needs TH but it cannot synthesize it, so TSH levels increase. TRH levels also increase accordingly (after all, without TRH, TSH cannot be released in the large amounts characteristic of iodine deficiency). Because TSH levels are higher than normal, the thyroid increases activity significantly, and develops a goiter. This condition is called hypothyroidism.
Hyperthyroidism occurs when there is an excess of TH release and activity. The most common cause of hyperthyroidism is Graves' disease, which is an autoimmune disorder. In this condition, autoantibodies against the TSH receptor on the thyroid gland cause excessive production of TH, resulting in higher-than-normal metabolic activity. Patients with hyperthyroidism also suffer from goiter.
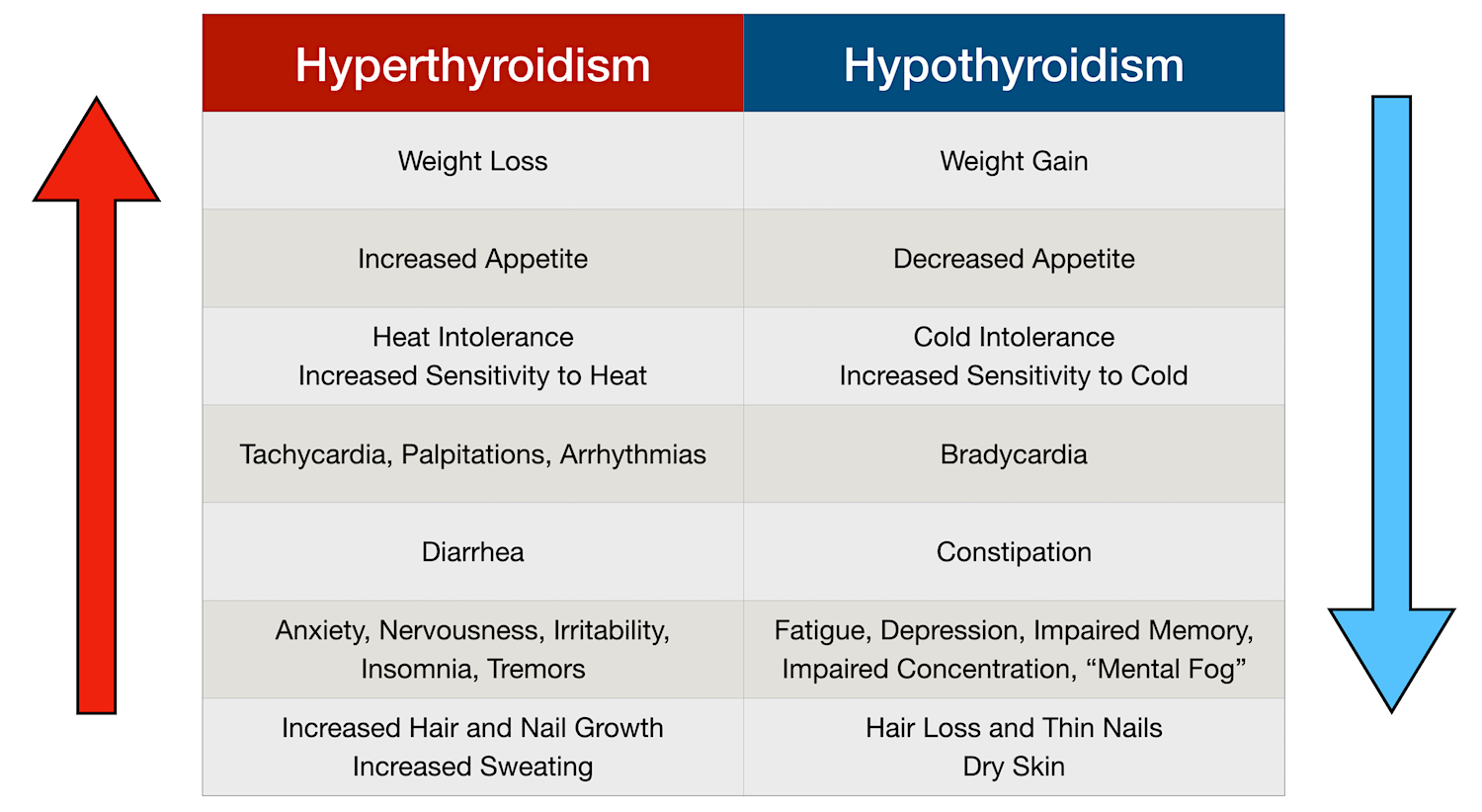
Symptoms of hyper and hypothyroidism include the following:
Because the thyroid hormones control the essential function of metabolism, it is important to maintain euthyroidism.
Here are some resources that helped me understand these concepts:
https://en.wikipedia.org/wiki/Thyroglobulin - A short Wikipedia article about the functions of Tg.
https://www.pennmedicine.org/for-patients-and-visitors/patient-information/conditions-treated-a-to-z/hyperthyroidism-overactive-thyroid - Article about hyperthyroidism.
https://pubmed.ncbi.nlm.nih.gov/9534029/ - In-depth review of the pathogenesis of Graves' disease.
https://youtu.be/5aq_rxTbtws - Ninja Nerd video overview of thyroid hormone function.